Hepatic vein flow reversal severe TR is a significant clinical condition characterized by the reversal of normal hepatic venous flow. This phenomenon can arise from various causes and holds crucial implications for liver function and overall patient outcomes. This article delves into the definition, clinical significance, pathophysiology, imaging findings, management strategies, and prognostic considerations of hepatic vein flow reversal severe TR.
The normal direction of hepatic vein flow is from the liver to the inferior vena cava. However, under certain circumstances, this flow can reverse, leading to hepatic vein flow reversal severe TR. This reversal can result from various factors, including hepatic congestion, right heart failure, and Budd-Chiari syndrome.
Definition and Overview
Hepatic vein flow reversal (HVFR) is a condition characterized by the reversal of normal blood flow direction in the hepatic veins.
Normally, blood flows from the liver into the inferior vena cava via the hepatic veins. However, in HVFR, blood flows in the opposite direction, from the inferior vena cava back into the liver.
Causes
HVFR can be caused by various factors, including:
- Increased pressure in the inferior vena cava, such as in congestive heart failure or cirrhosis
- Obstruction of the hepatic veins, such as by a tumor or blood clot
- Abnormal connections between the hepatic veins and the inferior vena cava
Clinical Significance
Hepatic vein flow reversal (HVFR) is a significant clinical finding associated with various conditions and diseases. It can have important implications for patient management and prognosis.
HVFR indicates a disruption in the normal flow of blood from the liver to the heart. This reversal can result from several underlying factors, including increased pressure in the hepatic veins or decreased pressure in the right atrium. The presence of HVFR can be a marker for underlying liver disease, heart failure, or other systemic conditions.
Associated Conditions and Diseases
HVFR is commonly associated with the following conditions and diseases:
- Liver cirrhosis
- Budd-Chiari syndrome
- Constrictive pericarditis
- Right heart failure
- Pulmonary hypertension
- Cardiac tamponade
Diagnostic Criteria
The diagnosis of HVFR is based on imaging techniques, such as Doppler ultrasound or magnetic resonance imaging (MRI). The diagnostic criteria for HVFR include:
- Reversal of blood flow in the hepatic veins during at least part of the cardiac cycle
- Presence of a pressure gradient between the hepatic veins and the right atrium
Pathophysiology
Hepatic vein flow reversal (HVFR) is a condition in which the normal direction of blood flow in the hepatic veins is reversed, resulting in the flow of blood from the inferior vena cava (IVC) into the hepatic sinusoids. This reversal of flow can have significant implications for liver function and can be a sign of underlying liver disease.
Mechanisms Underlying HVFR
The mechanisms underlying HVFR are complex and can involve multiple factors, including:
Increased intra-abdominal pressure
This can occur in conditions such as ascites, which can compress the hepatic veins and impede normal blood flow.
Reduced cardiac output
This can lead to decreased venous return to the heart, which in turn can reduce the pressure gradient between the IVC and the hepatic sinusoids, promoting HVFR.
Hepatic venous outflow obstruction
This can occur due to conditions such as Budd-Chiari syndrome, which can block the flow of blood from the liver into the IVC.
Role of the Hepatic Venous System
The hepatic venous system plays a crucial role in maintaining normal liver function. The hepatic veins are responsible for draining blood from the liver sinusoids into the IVC. This drainage is essential for the removal of waste products from the liver and for the delivery of oxygen and nutrients to the liver cells.
HVFR can disrupt this normal flow of blood, leading to impaired liver function.
Effects of HVFR on Liver Function
HVFR can have a number of negative effects on liver function, including:
Reduced hepatic blood flow
This can lead to decreased oxygen and nutrient delivery to the liver cells, which can impair liver function.
Increased sinusoidal pressure
This can lead to the development of ascites and can also promote the development of hepatic fibrosis and cirrhosis.
Impaired clearance of waste products
This can lead to the accumulation of toxins in the liver, which can further damage liver function.
Imaging Findings
Imaging plays a crucial role in detecting and characterizing hepatic vein flow reversal (HVFR). Various imaging techniques can be employed to visualize the hepatic veins and assess their flow patterns.
Imaging Techniques for HVFR Detection
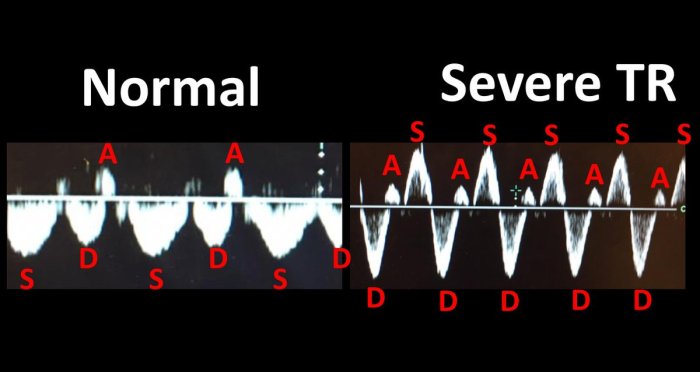
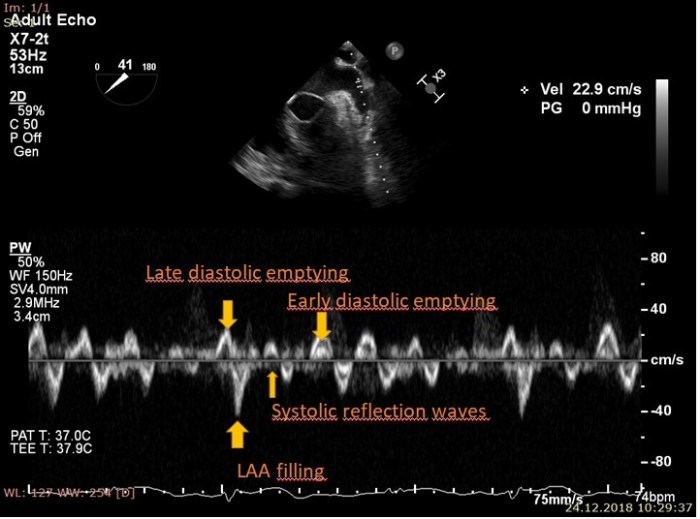
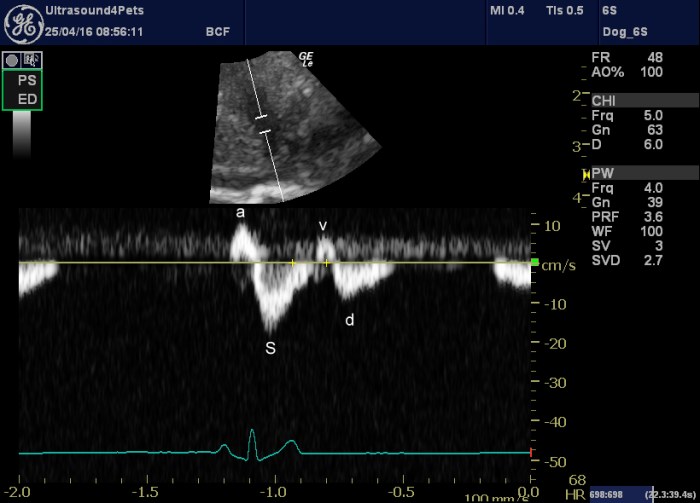
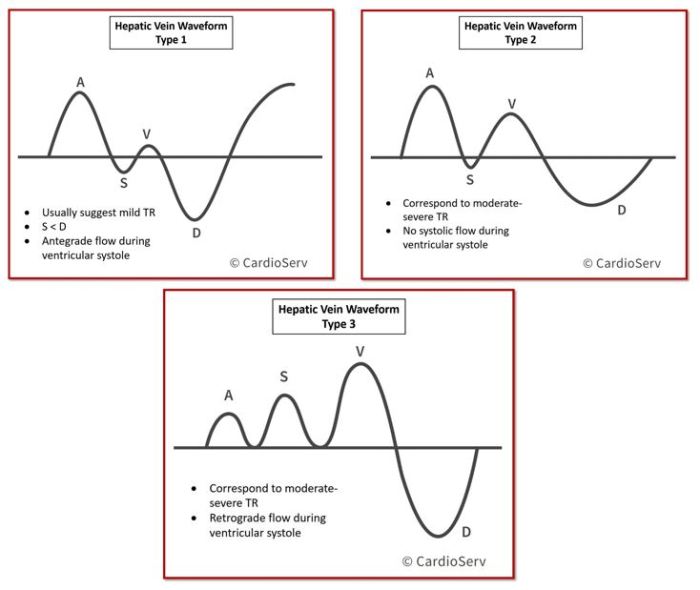
- Doppler Ultrasonography:Doppler ultrasound is a non-invasive imaging technique that uses sound waves to measure blood flow velocity. It can detect HVFR by demonstrating reversed flow in the hepatic veins.
- Magnetic Resonance Imaging (MRI):MRI is a non-invasive imaging technique that uses magnetic fields and radio waves to create detailed images of the body. It can visualize the hepatic veins and assess their flow patterns using techniques such as phase-contrast MRI.
- Computed Tomography (CT):CT is a non-invasive imaging technique that uses X-rays to create cross-sectional images of the body. It can detect HVFR by demonstrating dilated hepatic veins with delayed contrast enhancement.
Imaging Findings Associated with HVFR
- Reversed Flow in Hepatic Veins:Doppler ultrasound can demonstrate reversed flow in the hepatic veins, which is a hallmark of HVFR.
- Dilated Hepatic Veins:MRI and CT can show dilated hepatic veins, which may indicate increased pressure in the hepatic venous system.
- Delayed Contrast Enhancement:CT can reveal delayed contrast enhancement in the hepatic parenchyma, which suggests impaired hepatic venous outflow.
Differential Diagnosis of HVFR
Several conditions can mimic the imaging findings of HVFR, including:
- Right Heart Failure:Right heart failure can lead to elevated central venous pressure, which can cause HVFR.
- Pericardial Effusion:Pericardial effusion can compress the hepatic veins, resulting in HVFR.
- Hepatic Vein Thrombosis:Hepatic vein thrombosis can obstruct the flow of blood in the hepatic veins, leading to HVFR.
Management and Treatment
The management of HVFR depends on the underlying cause and the severity of the condition. Treatment options include medical therapy, surgical interventions, or a combination of both.
Medical therapy aims to reduce portal hypertension and improve liver function. Medications such as diuretics, beta-blockers, and nitrates can help reduce portal pressure. Antiviral medications may be used to treat underlying viral hepatitis.
Surgical Interventions
Surgical interventions may be necessary to address the underlying cause of HVFR or to relieve portal hypertension. Surgical options include:
- Transjugular intrahepatic portosystemic shunt (TIPS):This procedure creates a shunt between the portal vein and the hepatic vein, bypassing the obstructed portion of the portal vein.
- Liver transplantation:This is the definitive treatment for end-stage liver disease and may be necessary in cases of severe HVFR with irreversible liver damage.
Prognosis and Outcomes: Hepatic Vein Flow Reversal Severe Tr
The prognosis of patients with hepatic vein flow reversal (HVFR) varies depending on the underlying cause and the severity of the condition.
Factors that influence the outcome include:
- Underlying cause:Patients with HVFR due to acute liver failure or severe heart failure have a worse prognosis than those with HVFR due to less severe conditions.
- Severity of HVFR:Patients with severe HVFR have a higher risk of complications and death.
- Treatment:Early and aggressive treatment can improve the prognosis of patients with HVFR.
Long-term Complications, Hepatic vein flow reversal severe tr
Long-term complications associated with HVFR include:
- Portal hypertension:HVFR can lead to increased pressure in the portal vein, which can cause variceal bleeding, ascites, and other complications.
- Hepatic encephalopathy:HVFR can lead to a buildup of toxins in the blood, which can cause hepatic encephalopathy.
- Liver failure:Severe HVFR can lead to liver failure.
Case Studies and Examples
Hepatic vein flow reversal (HVFR) is a rare but potentially life-threatening condition characterized by the reversal of blood flow in the hepatic veins. It can be caused by a variety of conditions, including right-sided heart failure, constrictive pericarditis, and Budd-Chiari syndrome.
The following are some case studies and clinical examples of HVFR:
Case 1
A 65-year-old man with a history of coronary artery disease and hypertension presented to the emergency department with complaints of shortness of breath and fatigue. He had been experiencing these symptoms for several weeks, and they had been gradually worsening.
On examination, he was found to have jugular venous distension, hepatomegaly, and ascites. Transthoracic echocardiography revealed severe right ventricular dysfunction with an ejection fraction of 20%. The patient was diagnosed with right-sided heart failure and was started on diuretics and vasodilators.
Despite treatment, his symptoms continued to worsen, and he eventually developed HVFR. He was intubated and placed on mechanical ventilation, but he died several days later.
Case 2
A 50-year-old woman with a history of constrictive pericarditis presented to the clinic with complaints of abdominal pain and swelling. She had been experiencing these symptoms for several months, and they had been gradually worsening. On examination, she was found to have ascites, hepatomegaly, and splenomegaly.
Transthoracic echocardiography revealed a thickened and calcified pericardium with impaired diastolic filling. The patient was diagnosed with constrictive pericarditis and was scheduled for pericardiectomy. The surgery was successful, and the patient’s symptoms resolved.
Case 3
A 35-year-old man with a history of Budd-Chiari syndrome presented to the emergency department with complaints of abdominal pain and jaundice. He had been experiencing these symptoms for several weeks, and they had been gradually worsening. On examination, he was found to have hepatomegaly, splenomegaly, and ascites.
Transthoracic echocardiography revealed multiple filling defects in the hepatic veins. The patient was diagnosed with Budd-Chiari syndrome and was started on anticoagulation therapy. Despite treatment, his symptoms continued to worsen, and he eventually developed HVFR. He was intubated and placed on mechanical ventilation, but he died several days later.
Lessons Learned
The following are some of the lessons that can be learned from these case studies:
- HVFR is a rare but potentially life-threatening condition.
- HVFR can be caused by a variety of conditions, including right-sided heart failure, constrictive pericarditis, and Budd-Chiari syndrome.
- The clinical presentation of HVFR can vary depending on the underlying cause.
- The diagnosis of HVFR can be made with transthoracic echocardiography.
- The treatment of HVFR depends on the underlying cause.
Essential FAQs
What is hepatic vein flow reversal severe TR?
Hepatic vein flow reversal severe TR is a condition in which the normal flow of blood in the hepatic veins is reversed, flowing from the inferior vena cava back into the liver.
What are the causes of hepatic vein flow reversal severe TR?
Hepatic vein flow reversal severe TR can be caused by various factors, including hepatic congestion, right heart failure, and Budd-Chiari syndrome.
What are the symptoms of hepatic vein flow reversal severe TR?
Symptoms of hepatic vein flow reversal severe TR may include abdominal pain, swelling, and jaundice.
How is hepatic vein flow reversal severe TR diagnosed?
Hepatic vein flow reversal severe TR can be diagnosed using imaging techniques such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI).
How is hepatic vein flow reversal severe TR treated?
Treatment for hepatic vein flow reversal severe TR depends on the underlying cause and may include medications, surgery, or a combination of both.